http://savvywillingandable.wordpress.com/2013/09/25/the-biopsychosocial-model-explained/
HOW IT WAS THEN, HOW IT IS NOW
In the past, the biomedical model was the most widely used approach by healthcare professionals in the management of patients with chronic low back pain.
The focus of this model was the idea that pain experienced by a patient is entirely due to harm on the body tissues.
Disregarding other psychological, social and economic factors that also affects a person as a whole (Bendelow, 2013). It remained so until years later when this model was criticised by George Engel.
The biomedical model was critiqued for not being sufficient enough in the course of managing patients. This criticism gave rise to the current biopsychosocial model.
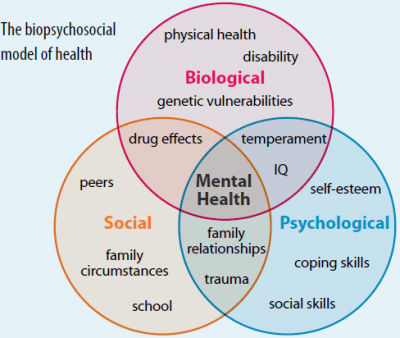
The biopsychosocial model was coined with the notion that regarding a person’s painful experience, there is more than just the alteration of biological factors but also the coexistence of psychological and social factors (Engel, 1977).
I first heard about the biopsychosocial model in the clinical reasoning module of my undergraduate studies. I clearly remember the lecturer saying, “pain is not always an issue in the tissue”.
If this is the case? why isn’t the biopsychosocial model effectively practised in Tanzania? is there something wrong with the model itself?
THE ACHILLES HEEL
Despite being important and supported by recent research, just like the biomedical medical, the biopsychosocial model has also been criticised in a number of ways in the developed countries in America and Europe utilising this model.
Many of the criticisms relate to the situation in Tanzania. One of the limitations of the biopsychosocial model is the fact that, it is difficult to be practised in a clinical setting as it demands time to do so (Herman J, 2005).
With regard to the imbalance between the number of health care providers and patients seeking medical care in Tanzania, it becomes difficult to apply the model in practice.
The biopsychosocial model highlights psychological, emotional and lifestyle/ social factors as the cause of a painful condition.
Nevertheless, this model does not foster common language among clinicians of which among the factors is the most likely contributor of a painful experience (Freudenreich et al, 2010).
This leaves clinicians to lean on their own understanding and clinical reasoning in decision making about the cause of pain to the patient in relation to the dimensions of the biopsychosocial model. (Searight, 2016).
This also appears be so in Tanzania thus accounting for the variations of treatment from clinician to clinician and from clinic to clinic.
Not only that but also, some researchers have argued that it is also rather hard to measure the effectiveness of the biopsychosocial model (Ghaemi, 2010).
In Tanzania, this is also evident due to the scarcity of high-quality research about the biopsychosocial model per se as well as conditions such as low back pain that follow its framework (Tatsumi et al, 2019).
With these limitations of the model? does it mean it’s best to leave the situation in Tanzania as it is?
Inspite of the model’s limitations, there has been evidence that the biopsychosocial model is effective in the management of patients with chronic low back pain.
This is because, it depicts the association between psychological and social factors hence encourages patients to actively take charge in relieving their pain (Kusnanto et al, 2018).
But then, what is the rationale of the biopsychosocial model?
REFERENCES:
Bendelow, G. (2013) ‘Chronic pain patients and the biomedical model of pain’, Virtual Mentor, 15(5), pp. 455–459. doi: 10.1001/virtualmentor.2013.15.5.msoc1-1305.
Engel, G. L. (1989) ‘The need for a new medical model: A challenge for biomedicine’, Journal of Interprofessional Care. doi: 10.3109/13561828909043606.
Freudenreich, O.; Kontos, N.; Querques, J. (2010) ‘The Muddles of Medicine: A Practical, Clinical Addendum to the Biopsychosocial Model. Psychosomatics’, 51, 365–369.
Herman, J. (2005) ‘The Need for a Transitional Model: A Challenge for Biopsychosocial Medicine?’ Fam. Syst. Health Spec. Issue Curr. State Biopsychosoc., 23, 372–376.
Tatsumi, M., Mkoba, E.M., Suzuki, Y. et al. (2019) ‘Risk factors of low back pain and the relationship with sagittal vertebral alignment in Tanzania. BMC Musculoskelet Disord 20, 584 (2019 doi:10.1186/s12891-019-2953-x
Kusnanto, G. and Supangat A (2018) ‘The design of IT development based on EA model for Islamic boarding school’, in Proceedings of the 3rd International Conference on Informatics and Computing, ICIC . doi: 10.1109/IAC.2018.8780460.
Searight, H.R. The Biopsychosocial Model (2016): “Reports of My Death Have Been Greatly Exaggerated.”. Cult. Med. Psychiatry 2016, 40, 289–298.
Ghaemi, S.N. (2019) ‘The rise and fall of the biopsychosocial model. Br. J. Psychiatry’, 195, 3 Kusnanto, G. and Supangat A (2018) ‘The design of IT development based on EA model for Islamic boarding school’, in Proceedings of the 3rd International Conference on Informatics and Computing, ICIC 2018. doi: 10.1109/IAC.2018.8780460.
Kusnanto, G. and Supangat A (2018) ‘The design of IT development based on EA model for islamic boarding school’, in Proceedings of the 3rd International Conference on Informatics and Computing, ICIC 2018. doi: 10.1109/IAC.2018.8780460.
like your writing style 👍
LikeLiked by 1 person
Thanks, I hope you liked the content as well!
LikeLike